Vascular and Endovascular
Vascular services investigate and manage conditions affecting the major blood vessels of the body (arteries and veins). Arteries take oxygen rich blood to the various tissues and organs, whilst veins return it to the heart once the oxygen has been removed. Once the blood picks up more oxygen by circulating through the lungs, the cycle is repeated. Disorders of both arteries and veins can cause symptoms which prompt referral to the vascular service.
Symptoms range from varicose veins, which can normally be treated simply on a daycase basis often under local anaesthetic, to blockages or bursting of major arteries. Blocked arteries can cause a reduction of the blood flow to an organ or limb, and may require surgical repair or replacement of the affected artery to prevent serious damage to, or loss of, the organ or limb.
Many vascular conditions can now be treated in the x-ray room, without recourse to major surgery. This is known as “endovascular surgery”, and involves treating the artery or vein from inside. This technique is less invasive than surgery, but is not always appropriate.
Our service covers a population of 1.5million people from Barrow, Kendal, Lancaster, Blackpool and Wigan. We provide both outpatient clinics and day case surgery across this area.
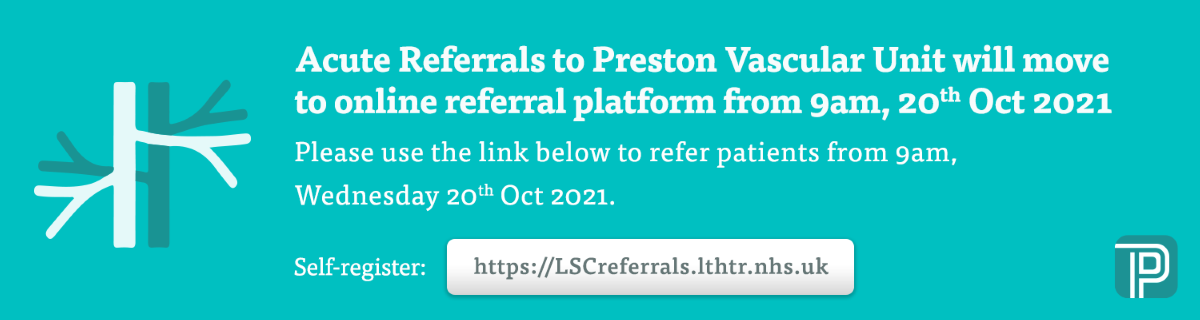
- Vascular Referrals and Advice
- Becoming a Specialist Centre
 In 2012 The Vascular Society of Great Britain and Ireland published The Provision of Services for Patients with Vascular Disease which stated: “Our primary objective is to provide all patients with vascular disease with the lowest possible elective and emergency morbidity and mortality rates in the developed world. To achieve this we will need to modernise our service and deliver world class care from a smaller number of higher volume hospital sites.”
In 2012 The Vascular Society of Great Britain and Ireland published The Provision of Services for Patients with Vascular Disease which stated: “Our primary objective is to provide all patients with vascular disease with the lowest possible elective and emergency morbidity and mortality rates in the developed world. To achieve this we will need to modernise our service and deliver world class care from a smaller number of higher volume hospital sites.”Arterial Partners
In October 2013, following a major review of vascular services in Lancashire and Cumbria, it was recommended that Lancashire Teaching Hospitals be designated as one of the major Vascular Interventional Centres in the country with the centre being based at Preston.
The agreed footprint of services is a “hub and spoke” arrangement, with vascular consultants in neighbouring hospitals in Morecambe Bay, Blackpool and Wrightington, Wigan and Leigh bringing all in-patient and emergency arterial work to the centre at Preston, whilst keeping day case and out-patient work locally. This is to ensure patients receive the best care possible but as close to home as possible.
The Arterial Partners Network is now in a position to centralise all major arterial services into the Centre based at Lancashire Teaching Hospitals Trust (LTHT) with full support of the three arterial partner hospitals. The new centre will cover a population of approximately 1.5 million.
The launch date of the service was January 2015 and there is a phased implementation of the centralised service taking place as follows:
- Out of Hours Surgery rota for all four partner trusts July 2014
- Trust 1 (Morecambe Bay)emergencies Jan 2015
- Trust 1 (Morecambe Bay)elective March 2015
- Trust 2 (Wrightington, Wigan and Leigh) emergencies June 2015
- Trust 2 (Wrightington, Wigan and Leigh) elective Sept 2015
- Trust 3 (Blackpool) emergencies Jan 2016
- Trust 3 (Blackpool) elective March 2016
There are 10 vascular surgeon consultants across the partnership, using a consultant of the week system and a separate out of hours on call rota. This means that the consultant of the week deals with all emergencies cases arriving at the centre in working hours, liaises with other hospital sites for patient transfers, undertakes a full ward round each day to review and discharge patients in a timely manner and acts as a consistent point of care for patients. The out of hours rota caters for emergencies which require immediate treatment overnight or at the weekend. This design ensures a consistently safe and high quality service for patients across the partnership.
- Conditions We Treat
Problems with the circulation to the limbs
“Peripheral arterial disease” is a condition in which a fatty deposit (atheroma) builds up within the arteries one or more limbs, most commonly affecting the leg. This leads to narrowing or blockage of the artery, which in turn leads to impairment of the blood supply to the affected limb. This can cause pain when walking (intermittent claudication), or, more seriously, to severe circulation problems ultimately requiring intervention to prevent amputation. Many such blockages can be managed by endovascular means, by stretching the artery or inserting a “stent” (a wire mesh cylinder to help keep the artery open), although some will require a surgical operation to “bypass” the blocked artery.
Narrowing of the Internal Carotid Artery
Atheroma can also build up in the arteries supplying the brain (the internal carotid arteries). This is known to be a common cause of stroke, and often presents with a temporary “ministroke” more properly referred to as a Transient Ischaemic Attack. This takes the form of temporary weakness affecting one arm, one leg, or both an arm and a leg (but both on the same side of the body). Alternatively, there may be temporary speech difficulties or transient vision loss in one eye. Such an event does suggest that there is a high risk of imminent stroke and requires urgent investigation and treatment. Whilst treatment is often by medication and changes in lifestyle, more severe narrowings are treated by an operation to remove the diseased inner layer from the artery (carotid endarterectomy).
Abdominal aortic aneurysm
An aneurysm is a weakening of an artery due to deposition of a fatty deposit (atheroma) within its wall. This causes stretching and ballooning and renders the artery in danger of bursting. This most commonly affects the main artery in the abdomen (the abdominal aorta). Aneuryms can be repaired by an open operation to replace the weakened artery, or, in many cases, insertion of an artificial artery (stent-graft) by endovascular means (ie from inside the artery through small groin incisions). This latter procedure is known as EVAR (endovascular aneurysm repair), and is now the commonest method for repairing aortic aneurysms.
Varicose Veins
This is an extremely common condition which results in distension of the superficial veins of the leg due to faulty one way valves, impairing the vein's ability to drain the blood adequately. This can cause leg pain, skin changes or even ulcer formation. Most varicose veins nowadays can be treated by a simple procedure normally done under local anaesthetic.
Leg Ulcers
Leg ulcers are common, particularly in elderly people, and may be due to problems with the veins, the arteries or both. Whilst many ulcers can be managed at home, some require further investigations and surgery or endovascular treatment to help the ulcer to heal.
Vascular Trauma
Injury to major blood vessels is a serious potential complication of major road traffic accidents which can result in bleeding or impairment of blood flow to an organ or limb. This often requires surgery or endovascular treatment to repair the damaged artery or vein.
- Development of the Hybrid Theatre
Hybrid theatre
 A hybrid theatre is a combined operating theatre and interventional radiology suite. The hybrid theatre can function as either a conventional operating theatre or as a radiology facility but crucially allows intra operative and post-operative imaging and intervention, and overcomes many of the limitations of standard facilities.
A hybrid theatre is a combined operating theatre and interventional radiology suite. The hybrid theatre can function as either a conventional operating theatre or as a radiology facility but crucially allows intra operative and post-operative imaging and intervention, and overcomes many of the limitations of standard facilities.Vascular services include the treatment of aneurysm and other abnormal blood vessels, limb ischaemia, carotid artery disease, peripheral and visceral arterial disease, thoracic outlet surgery and venous disease. Interventional radiology for vascular disease involves a range of minimally invasive image-guided techniques for stenting and repair of vessels. Many endovascular operations require surgical input, and there are progressively increasing numbers of procedures which are part surgical and part endovascular. Such procedures require full operating theatre specifications with high quality imaging facilities.
 Within vascular services there has been a shift in the treatment of Abdominal Aortic Aneurysm (AAA) from Open Repairs to Endovascular Repair (EVAR), where possible and appropriate. Open Repair involves cutting open the abdomen to replace the aneurysm with an artificial piece of artery – a graft. This is a major operation and carries some risk. EVAR involves inserting a stent -graft within the aneurysm through smaller surgical groin incisions using X-rays to guide the graft into place. The advantage of this type of repair is that there is no open abdominal surgery. This technique is therefore safer than the traditional operation and the patient spends less time in hospital. There is always the potential to convert to open repair or perform an emergency bypass graft.
Within vascular services there has been a shift in the treatment of Abdominal Aortic Aneurysm (AAA) from Open Repairs to Endovascular Repair (EVAR), where possible and appropriate. Open Repair involves cutting open the abdomen to replace the aneurysm with an artificial piece of artery – a graft. This is a major operation and carries some risk. EVAR involves inserting a stent -graft within the aneurysm through smaller surgical groin incisions using X-rays to guide the graft into place. The advantage of this type of repair is that there is no open abdominal surgery. This technique is therefore safer than the traditional operation and the patient spends less time in hospital. There is always the potential to convert to open repair or perform an emergency bypass graft.Most interventional radiology suites (based in X-ray) are not designed to incorporate an anaesthetic machine and the additional staff required for a general anaesthetic procedure. Radiology suites often lack the positive pressure, air change cycling ability and environmental control of an operating theatre. Other issues include a lack of optimal lighting and suction facilities if an open surgical procedure is required. Although EVAR complications are rare (3.8%) it is possible that, with the increasing volume of endovascular cases, their complexity and the possibility of ruptured aneurysms during endovascular repair, the need for conversion to open repair may increase. Other procedures requiring a combined surgical and radiological approach, such as femoral endarterectomy and iliac angioplasty will also be undertaken in this setting.
A hybrid theatre is the required option for this complex work with permanent imaging equipment. Theatres are built to allow rapid decontamination cleaning and to promote the optimum sterile environment. The use of portable imaging equipment within an operating theatre may cause a threat to the sterility. In addition the MHRA have advised against the use of mobile intensifiers for EVAR.
There will also be an opportunity for other procedures to be accommodated within the Hybrid Theatre such as complicated obstetric procedures (placental invasion deliveries) and major trauma cases.
- Interventional Radiology
Treatment for vascular (circulation) conditions
In the past, patients with vascular conditions always needed conventional open surgery. Nowadays many vascular conditions can be treated with key hole surgery under x-ray using a specialist technique called interventional radiology. Interventional radiology involves making small cuts in the body’s vessels and using x-rays and scans to insert and manoeuvre tiny devices to treat the problem.

Interventional radiology is a less invasive, safer procedure than traditional open surgery. It helps patients recover more quickly, and requires specialist skills and facilities. Open surgery is still the best treatment for some conditions including complex disorders and should always be done by specialist vascular surgeons.
Nowadays, not every hospital provides treatment for every condition. Increasingly, less common and complex treatment is provided in fewer centres of excellence, which have specialist facilities, where staff can develop expertise and experience. Organising care for less common and often serious and complex conditions in this way improves recovery and saves lives.
In Lancashire and South Cumbria patients with minor vascular conditions receive care and treatment in their local hospital. Patients with severe vascular conditions, including life-threatening emergencies, are treated in the region’s Vascular Centre, at Royal Preston Hospital. Patients may be transferred to their local hospital for further care following treatment of a severe vascular condition at the Vascular Centre.
Work is currently underway to build a new specialist operating theatre at the Vascular Centre at Royal Preston Hospital, and additional staff are being recruited. See our latest jobs for opportunities to work in the Vascular Centre.
- Our Consultants
The consultant vascular surgeons work closely with the rest of the regional multi-disciplinary team in the vascular service to provide accurate assessment diagnosis and treatment of all vascular conditions. They offer a full range of vascular interventions both surgical and radiological.
Consultants
Click on a consultant to see more information.
- Our Wider Team
Consultant Interventional Radiologists
The consultant interventional radiologists work closely with the rest of the regional multi-disciplinary team in the vascular service to provide expert diagnosis and interventional radiology treaments for vascular conditions.
Alistair Craig
Job Title: Consultant in Interventional and Diagnostic Radiology
Department: Radiology
Telephone Number: 01772 522516
Primary Medical Qualification: MB ChB (Manchester)
Other Qualifications: FRCR (London) Bsc Hons (Leeds)
Year of Registration: 2000
GMC Number: 4707239
Career History: House Officer in Medicine, Hope Hospital. House Officer in Surgery, North Manchester General Hospital. Senior House Officer Medicine, Royal Preston Hospital. Senior House Officer Medicine, Hope Hospital. Specialist Registrar Radiology, North West Training Scheme
Specialist Areas: Vascular and non-vascular intervention; body CT and MRI ultrasound (vascular and general)
Specialists Interests: Fibroid embolisation; EVAR dialysis; access and AV fistula salvage; trauma radiology and intervention
Research Interests: Undertaking MSc in clinical education (University of Edinburgh)
Clinics: Radiology Outpatient Clinic
Languages Spoken: English
Awards and Prizes:
Best First Time Presenter UKRC (2005)
Poster Prize BSIR (2004)
Medical Futures Award (2007)Stephen D'Souza
Tom Houghton
Choong Poon
James Simpson
Job Title: Consultant Interventional Radiologist
Department: Radiology/Imaging
Telephone Number: 01772 524169
Primary Medical Qualification: BM BS
Other Qualifications: B Med. Sci., MRCS, FRCR
Year of Registration: 1998
GMC Number: 4539274
Career History: Qualified Nottingham University 1998, Basic Surgical Training Rotation, Hull and East Yorkshire NHS Foundation Trust 1999-2002, Specialist Registrar Rotation Radiology, Hull and East Yorkshire NHS Foundation Trust 2002-2007, Consultant Interventional Radiologist, Calderdale and Huddersfield NHS Foundation Trust 2007-2014, Consultant Interventional Radiologist, Lancashire Teaching Hospitals NHS Foundation Trust 2014- present
Specialist Areas: Endovascular treatment of peripheral vascular disease, Endovascular aortic aneurysm repair (EVAR), Uterine Fibroid Embolisation (UFE)
Consultant Vascular Anaesthetists
Alex Bonner
Job Title: Consultant Anaesthetist with specialist interest in vascular anaesthesia. Honorary Lecturer, University of Manchester
Primary Qualification: MBChB (Hons) 2005 University of Leicester
Other Qualifications: FRCA PGDip Med Ed
Year of Entry onto Specialist Register: 2015
GMC: 6118754
Career History: Postgraduate training in Leicester and North West Deanery. Group of Anaesthetists in Training (GAT) committee member. Experience of practising anaesthesia in Uganda and India. 1 year fellowship in education and simulation at University of Manchester. Appointed to Lancashire Teaching Hospitals February 2015
Specialist areas: Vascular anaesthesia and medical education
Specialist interests: Peri-operative management of the high risk surgical patient. Improving training in vascular anaesthesia. Active as a mentor to doctors of all grades and specialities
Research interests: Use of mobile technology in medical education
Martin Letheren
Job Title: Consultant Anaesthetist
Primary Qualification: MBChB BSc
Other Qualification: FRCA
Year of Registration: 1989
GMC: 3305739
Career History: St Andrews and Manchester Medical schools graduating 1989. Anaesthetic training within the North West. Appointed as consultant to Royal Preston Hospital 1997.
Specialist Areas: Anaesthesia for vascular, neurosurgery, spinal surgery and paediatric dental surgery. Extensive experience in hospital management and education. Presently Royal College Tutor and NCAS assessor.
Research Interests: Decision making in the work place and patient safety.
Kaushal Mishra
Jennifer OldridgeThomas O'Neill
Job Title: Consultant Anaesthetist with a special interest in Anaesthesia for Vascular and Trauma Surgery
Department: Department of Anaesthetics
Telephone Number: 01772 522555
Primary Medical Qualification: MBBS
Other Qualifications: MA, FCARCSI
Year of Registration: 2001
GMC Number: 6028115
Career History: Qualified University of London, 2001
Specialist Registrar training in Anaesthesia, North West Deanery,
Fellowship in Regional Anaesthesia and Acute Pain, North West Deanery
Consultant at Lancashire Teaching Hospitals NHS Foundation Trust since October 2013Specialist Areas:
Anaesthesia for Vascular and Trauma Surgery
Specialist Interests:
Lead Vascular Anaesthetist
Preoperative assessment including Cardiopulmonary Exercise Testing
Regional Anaesthesia
Chair of the Hospital Transfusion Committee
Languages Spoken: English
Specialist Vascular Nurse Team
Melissa Hughes
Melissa completed her diploma in adult nursing in 2002. She initially worked on a general surgical ward and then the Surgical Assessment Unit. She has always had a passion for vascular surgery and wound management. Melissa joined the vascular team full time as a vascular specialist nurse in January 2009. Her role involves supporting vascular patients and their relatives from diagnosis of a vascular condition to treatment and follow up care. She also participates in nurse led clinics including: vascular assessment clinics, complex leg ulcer clinics and pre-operative assessment.
Ingrid SaulIngrid was appointed as a vascular specialist nurse in 2002 and completed a nursing diploma and a (BA Hons) degree in professional practice in 2003. During this time Ingrid has also gained qualifications in a specialist vascular course and leg ulcer management course. Once appointed she established the nurse led clinic's for the vascular patients. These include; the vascular assessment clinic, the pre-operative clinic, the leg ulcer clinic for complex wounds and the botox clinic for axillary hiperhidrosis. As part of the multi-disciplinary team, Ingrid provides advice, support and information for patients from diagnosis and throughout the patients care and she is passionate about maintaining a seamless service for our patients.
Interventional Radiology Nurse Team
Mary Donnelly
Job Title: Clinical Nurse Lead- Imaging and Interventional Radiology
Department: IMAGING
Telephone Number: 01772 522343/522974
Primary Nursing Qualification: Registered Nurse (NMC)
Other Qualifications: Diploma Nursing Studies, BsC (Hons) Nurse Practitioner
Year of Registration: 1993
GMC Number: 90E0161E
Career History: Staff Nurse Medicine, Staff Nurse Radiology, Sister Radiology, Clinical Nurse Specialist IR, Clinical Lead Imaging
Specialist Areas/Interests: Radiology Nursing, IR and Vascular Access, Chair of UK IR Nurses and Radiographers Society (SIRNR), Vascular Access
Sarah LockerSarah completed her diploma in adult nursing in 2006 and joined the Interventional Radiology team, here at Royal Preston straight from qualifying. Since then she has developed her skills and academic qualifications to progress into the role of clinical nurse specialist. She specialises in vascular and non-vascular interventional radiology caring for patients pre, post and peri-operatively. She has a particular interest in vascular access devices where she is involved in their insertion, care and management. She is currently studying at MSc level to become an Advanced Practitioner; her role will involve her performing pre-operative assessment prior to interventional radiology procedures, where she will clinically assess patients, prescribe best medical treatment and provide health promotion. As part of a multidisciplinary team, Sarah provides patients and their family/carers with advice, support and information in order to enhance their journey and promote seamless care.
Sharron Sanderson
Interventional Radiology Sister
Sharron qualified in 1998 and her first position was as a staff nurse in renal and haematology at Salford Royal Hospital, followed by gastroenterology and medical admissions at Dewsbury hospital, before joining the interventional radiology team at Salford Royal Hospital.
Sharron commenced employment at Lancashire Teaching Hospitals as a sister in 2006 to help with the induction of neuro intervention to the hospital. She now specialises in vascular and non-vascular interventional radiology, and on a daily basis is involved in the day to day running of the unit, as well as partaking in the pre assessment, pre, peri and post- operative care of the patients. Sharron is a learning disability champion and is also the lead for infection control and diabetes management for the directorate.
Interventional Radiographer Team
Elaine Hewitt
Vascular Ward and Theatre Managers
Emma Kevill
Eileen BurbridgeVascular MDT Co-ordinator
Christine McBride
Job Title: Vascular MDT Co-ordinator
Department: Vascular Surgery
Tel: 01772 522315
I have worked as a medical secretary at Lancashire Teaching Hospitals NHS Foundation Trust since 1988, both in General Surgery, and since 1994 specifically within Vascular Surgery. I have worked as the Vascular MDT Co-ordinator since 2013. The Vascular Network MDT meeting is composed of both clinical and medical professionals from different specialties within our Network (Blackpool/Preston/Morecambe Bay/Wigan).
My role is to prepare the list of patients to be discussed at the MDT Meeting and provide the relevant information upon which the MDT members can base their decision of the best treatment plan for vascular patients and document a formal record of the MDT’s recommendations so that this information is available to Consultants and other healthcare professionals who see patients. I am also responsible for liaising with other healthcare staff regarding any actions they need to take as a result of MDT decisions, for example, booking urgent out patient appointments and planning dates for operative procedures.
Middle grade doctors
Yousef Elhediny